- Introduction to Genital Papillomavirus
- What is Genital Papillomavirus?
- Prevalence and transmission
- Types of Genital Papillomavirus
- High-risk vs. low-risk strains
- Common strains and their effects
- Symptoms and Diagnosis
- Signs and symptoms
- Diagnostic procedures
- Treatment Options
- Medical interventions
- Home remedies and lifestyle changes
- Prevention Strategies
- Vaccination importance and efficacy
- Safe practices and risk reduction
- Impact on Health and Society
- Long-term consequences
- Societal impact and awareness
- Myths and Facts
- Common misconceptions
- Clarification of facts
- Support and Resources
- Support groups and counseling
- Reliable information sources
- Conclusion
Genital Papillomavirus: Understanding, Prevention, and Treatment
Introduction to Genital Papillomavirus
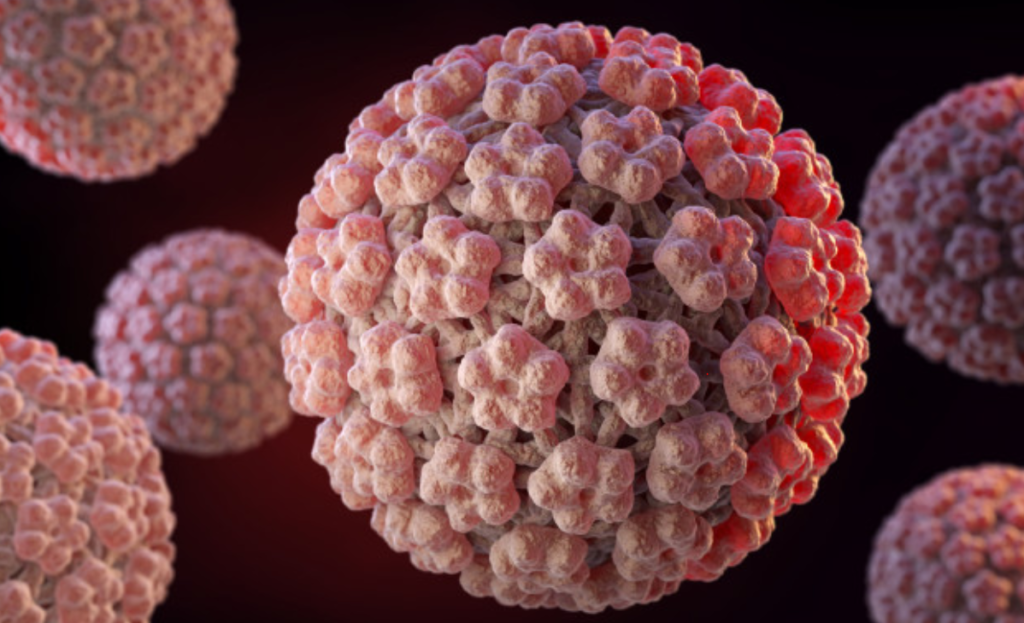
Genital Papillomavirus, commonly known as HPV (Human Papillomavirus), is a prevalent sexually transmitted infection affecting millions worldwide. It encompasses a diverse group of viruses known for their association with various conditions, predominantly causing warts on the genitals and in the throat or mouth.
Types of Genital Papillomavirus
This virus exhibits over 100 different strains, classified into high-risk and low-risk categories. High-risk strains, such as HPV 16 and 18, are notorious for their potential to lead to cervical cancer and other severe health issues. Conversely, low-risk strains often result in benign growths or warts.
Symptoms and Diagnosis
Identifying Genital Papillomavirus can be challenging as it often remains asymptomatic. However, symptoms may include genital warts, abnormal cell changes, or, in severe cases, cancers like cervical, anal, or throat cancer. Diagnosis typically involves physical examination, Pap tests, or HPV DNA tests.
Treatment Options
While there’s no cure for HPV itself, treatments aim to manage symptoms and associated health problems. Medical interventions like topical medications, surgical removal, or procedures to eliminate abnormal cells are common. Additionally, adopting a healthy lifestyle and boosting the immune system can aid in combating the virus.
Prevention Strategies
Preventing HPV primarily involves vaccination, a crucial step in protecting against various strains. Vaccination not only guards against cervical cancer but also reduces the risk of other HPV-related cancers. Alongside vaccination, practicing safe sex, using condoms, and limiting sexual partners can significantly lower transmission rates.
Impact on Health and Society
The long-term consequences of Genital Papillomavirus can be detrimental, leading to severe health complications and emotional distress. Moreover, the societal impact, including stigma and misinformation, contributes to challenges in HPV prevention and treatment.
Myths and Facts
Addressing misconceptions surrounding HPV is crucial. Common myths often lead to misunderstanding and misinformation. Clearing up these fallacies can help individuals make informed decisions about their sexual health and well-being.
Support and Resources
Numerous support groups and counseling services cater to individuals affected by HPV. These resources offer emotional support, information, and guidance, empowering individuals to navigate through their diagnosis and treatment journey effectively.
Conclusion
Genital Papillomavirus remains a prevalent and concerning health issue, emphasizing the importance of education, prevention, and access to reliable resources. By understanding the various aspects of HPV and adopting preventive measures, individuals can protect themselves and contribute to reducing its impact on society.
FAQs About Genital Papillomavirus
- Can HPV go away on its own? HPV can clear on its own in many cases, especially in healthy individuals with strong immune systems.
- Who is at risk of contracting HPV? Anyone who is sexually active can contract HPV, but certain behaviors may increase the risk.
- Is there a cure for HPV? While there’s no cure for HPV, treatments can manage symptoms and associated health problems.
- Is the HPV vaccine safe? Yes, extensive research supports the safety and efficacy of HPV vaccines in preventing various strains.
- How can I find reliable information about HPV? Reliable sources such as health department websites, medical journals, and healthcare professionals can provide accurate information about HPV.
- What are the potential complications of untreated HPV? Untreated HPV can lead to various health complications, including cervical, anal, or throat cancers, depending on the strain.
- Can you get HPV from non-sexual contact? While sexual contact is the most common mode of transmission, HPV can also spread through skin-to-skin contact.
- What age should one get vaccinated against HPV? The HPV vaccine is recommended for both boys and girls starting at the age of 11 or 12, but it can be administered up to age 26.
- How effective are condoms in preventing HPV? Condoms can reduce the risk of HPV transmission, but they may not fully protect against skin-to-skin contact.
- Is it safe to have sexual intercourse if diagnosed with HPV? It’s essential to discuss with a healthcare provider regarding sexual activity after an HPV diagnosis, considering individual circumstances and precautions.
Genital Papillomavirus: Understanding, Prevention, and Treatment
Introduction to Genital Papillomavirus
Genital Papillomavirus, commonly known as HPV (Human Papillomavirus), is a prevalent sexually transmitted infection affecting millions worldwide. It encompasses a diverse group of viruses known for their association with various conditions, predominantly causing warts on the genitals and in the throat or mouth.
Types of Genital Papillomavirus
This virus exhibits over 100 different strains, classified into high-risk and low-risk categories. High-risk strains, such as HPV 16 and 18, are notorious for their potential to lead to cervical cancer and other severe health issues. Conversely, low-risk strains often result in benign growths or warts.
Symptoms and Diagnosis
Identifying Genital Papillomavirus can be challenging as it often remains asymptomatic. However, symptoms may include genital warts, abnormal cell changes, or, in severe cases, cancers like cervical, anal, or throat cancer. Diagnosis typically involves physical examination, Pap tests, or HPV DNA tests.
Treatment Options
While there’s no cure for HPV itself, treatments aim to manage symptoms and associated health problems. Medical interventions like topical medications, surgical removal, or procedures to eliminate abnormal cells are common. Additionally, adopting a healthy lifestyle and boosting the immune system can aid in combating the virus.
Prevention Strategies
Preventing HPV primarily involves vaccination, a crucial step in protecting against various strains. Vaccination not only guards against cervical cancer but also reduces the risk of other HPV-related cancers. Alongside vaccination, practicing safe sex, using condoms, and limiting sexual partners can significantly lower transmission rates.
Impact on Health and Society
The long-term consequences of Genital Papillomavirus can be detrimental, leading to severe health complications and emotional distress. Moreover, the societal impact, including stigma and misinformation, contributes to challenges in HPV prevention and treatment.
Myths and Facts
Addressing misconceptions surrounding HPV is crucial. Common myths often lead to misunderstanding and misinformation. Clearing up these fallacies can help individuals make informed decisions about their sexual health and well-being.
Support and Resources
Numerous support groups and counseling services cater to individuals affected by HPV. These resources offer emotional support, information, and guidance, empowering individuals to navigate through their diagnosis and treatment journey effectively.
Conclusion
Genital Papillomavirus remains a prevalent and concerning health issue, emphasizing the importance of education, prevention, and access to reliable resources. By understanding the various aspects of HPV and adopting preventive measures, individuals can protect themselves and contribute to reducing its impact on society.
FAQs About Genital Papillomavirus
- Can someone be infected with HPV multiple times? Yes, it’s possible to get infected with different HPV strains over time, even after a previous infection clears.
- What is the link between HPV and cervical cancer? Certain high-risk HPV strains, if left untreated, can cause changes in cervical cells that may lead to cancer over time.
- Is there a test to determine if someone has HPV? Yes, tests like Pap smears or HPV DNA tests can detect the presence of HPV or abnormal cells.
- Can HPV affect fertility? In some cases, HPV may affect fertility, but it’s not a common occurrence. Consulting a healthcare provider is recommended for personalized guidance.
- How can I support someone diagnosed with HPV? Providing emotional support, encouraging seeking medical advice, and being non-judgmental can be crucial in supporting someone dealing with an HPV diagnosis.